Dental Implants 101: The Basics of an Implant
Replicating the Look and Feel of a Natural Tooth
Dental implants are a popular and effective solution for missing teeth, providing patients with a permanent and natural-looking replacement. At the core of a dental implant are three essential parts: the implant screw, abutment, and dental crown. Understanding these basic components is key to comprehending how dental implants function and can restore your smile and oral health. Let’s dive into Dental Implants 101 to explore this innovative tooth replacement option’s benefits, process, and maintenance.
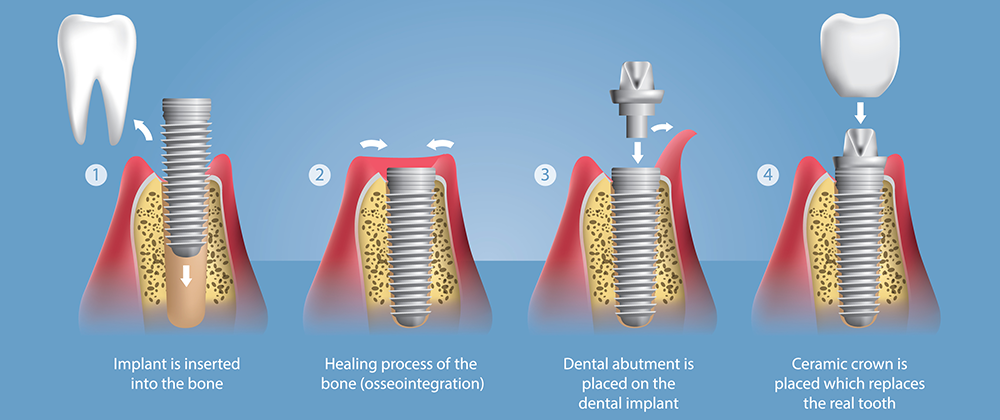
The three main components of a dental implant are the implant screw, abutment, and dental crown. The implant screw is a titanium post that is surgically placed into the jawbone to serve as a replacement for the tooth root. The abutment is a connector piece that is attached to the implant screw and supports the dental crown, which is the visible portion of the implant that resembles a natural tooth. These three components work harmoniously to provide a strong and lasting solution for missing teeth.
Dental Implants 101: Three Main Parts of an Implant
Implant Screw:
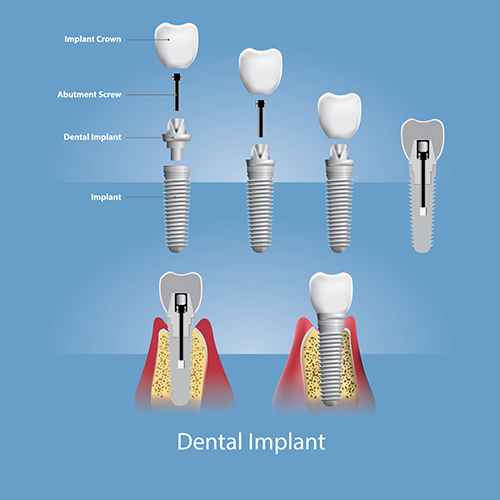
Anatomy of a Dental Implant: It has three essential components – the implant screw, abutment, and crown – working together to create a seamless and durable tooth replacement solution. 🦷✨ #DentalImplants #ToothReplacement #SmileConfidently
An implant screw is a small, biocompatible titanium post that serves as the foundation for a dental implant. It is surgically placed into the jawbone to mimic the function of a natural tooth root and provide stability for the replacement tooth. The implant screw fuses with the surrounding bone through a process called osseointegration, creating a strong and durable anchor for the dental implant. This integration helps ensure the long-term success and stability of the implant, allowing patients to eat, speak, and smile confidently.
Implant Abutment:
An implant abutment is a connector piece that is attached to the top of the implant screw. It serves as the link between the implant screw and the dental crown, providing support and stability for the replacement tooth. The abutment is typically made of titanium, zirconia, or another durable material and is custom-designed to fit the specific shape and size of the patient’s mouth. The abutment helps to secure the dental crown and ensures the proper fit and functionality of the dental implant.
Implant Crown:
An implant crown is the visible, artificial tooth attached to the abutment of a dental implant. It is typically made of porcelain or ceramic material and custom-made to match the shape, size, and color of the patient’s natural teeth. The implant crown is designed to function and look like a natural tooth, providing a seamless and aesthetically pleasing replacement for a missing tooth.
The main difference between the implant and regular crowns is how they are supported. A traditional crown is placed over an existing natural tooth, or a dental implant abutment is prepared to support the crown. In contrast, an implant crown is specifically made to be attached to the implant abutment, secured within the jawbone. This unique structure allows the implant crown to function independently without relying on surrounding teeth for support.
Overall, an implant crown offers a durable, long-lasting solution for missing teeth that closely mimics the look and function of natural teeth.
Dental Implants 101: Implant Solutions for Various Situations
Missing a Single Tooth:
The opportunity to extract a decayed tooth, install the implant, and construct a tooth directly onto the implant within one appointment is feasible, as is the process known as “Instant Implants” and “Instant Teeth.” This innovative approach offers the convenience of a faster treatment timeline, allowing patients to leave the dental clinic with a new tooth in place the same day. While not suitable for all cases, instant implants can be a viable option for some patients seeking a quick and efficient solution for tooth replacement.
Missing Multiple Teeth:
A fixed implant bridge procedure involves placing two or more dental implants in the jawbone to support a bridge of replacement teeth. These implants offer stability and help stimulate the surrounding bone, which can prevent bone loss that often occurs after tooth loss. By integrating with the jawbone through osseointegration, the dental implants act as artificial tooth roots, providing a solid foundation for the bridge.
Once the implants have fully fused with the bone, custom-made crowns are created to attach to them. These crowns are carefully crafted to match the color, shape, and size of the patient’s natural teeth, ensuring a seamless and natural-looking smile. The central crown of the bridge is positioned over the gums to fill in the gap left by the missing teeth, restoring both function and aesthetics.
Implant-supported bridges offer numerous advantages over traditional removable bridges, such as improved stability, longevity, and oral health benefits. With proper care and maintenance, these bridges can provide a lasting solution for multiple missing teeth, allowing patients to eat, speak, and smile confidently.
Missing all Your Teeth:
You only need 4 to 6 implants to support a bridge for all missing teeth, significantly minimizing the bone loss associated with traditional dentures. Dental implants offer a stable, prolonged solution, reducing the pain, discomfort, instability, and bone loss that people with dentures typically encounter. Another popular option is to opt for a denture anchored in place with implants.
Dental Implants 101: Alternative Options to Having Dental Implants
Partial dentures:
Partial dentures are a common and affordable solution for individuals with missing teeth; however, they come with drawbacks. While they can provide a quick fix for tooth loss, many people find them bulky and uncomfortable to wear. The constant movement and pressure exerted on the gums and remaining teeth can cause the partial dentures to become loose over time, leading to challenges and social awkwardness during meals and conversations.
One of the main disadvantages of partial dentures is the need to remove them at night for cleaning and maintenance. This daily routine can be cumbersome and inconvenient for many individuals, impacting their comfort and confidence. Furthermore, the pressure applied by the partial dentures on the underlying bone can contribute to bone loss in the jaw over time, affecting the overall oral health and stability of the remaining teeth.
In addition to these physical discomforts and inconveniences, partial dentures can have aesthetic implications. Visible metal clasps or hooks used to anchor the partial dentures in place may detract from the smile’s natural appearance, leading to self-consciousness and dissatisfaction with one’s oral aesthetics.
Overall, while partial dentures offer a temporary and cost-effective solution for missing teeth, their limitations in terms of comfort, stability, and impact on oral health may prompt individuals to explore more permanent and functional alternatives, such as dental implants or implant-supported bridges, for a more secure and natural-looking tooth replacement option.
Stick-on Bridges, aka Maryland Bridges:
Stick-on or Maryland bridges are dental restorations used in certain situations to replace missing teeth. These bridges are affixed to the adjacent teeth using metal or porcelain wings on the abutment teeth, providing a simple and minimally invasive option for tooth replacement. While stick-on bridges can temporarily fix the aesthetic and functional concerns associated with missing teeth, they have inherent limitations and drawbacks.
One of the main concerns with stick-on bridges is their susceptibility to dislodging or coming loose if excessive biting pressure is exerted. The reliance on the adjacent teeth for support means that the bridge’s stability may be compromised, especially when eating hard or sticky foods. This potential for movement can lead to discomfort, inconvenience, and anxiety for individuals wearing stick-on bridges, affecting their ability to eat and speak confidently.
Moreover, stick-on bridges do not address the issue of missing tooth roots, which play a crucial role in maintaining the health and integrity of the jawbone. Without the stimulation provided by a natural tooth root, the bone above the crown of the stick-on bridge may gradually diminish over time through a process known as bone resorption. This can result in a loss of bone density and volume in the jaw, leading to potential complications such as changes in facial structure, shifting of adjacent teeth, and increased susceptibility to fractures or injuries.
While stick-on bridges can be a convenient and cost-effective solution for some instances of tooth loss, individuals need to be aware of their limitations and potential risks. Regular dental check-ups and proper oral hygiene practices are crucial for monitoring the condition of stick-on bridges and addressing any concerns early on to ensure optimal oral health and function in the long run.
Fixed Bridges:
Fixed bridges are a traditional and commonly used dental restoration that can be an effective solution for replacing missing teeth. However, preparing for a fixed bridge involves removing a significant portion of the adjacent teeth to create space for the bridge to be placed. This process typically requires a high-speed drill, which can result in the removal of healthy tooth structure and potential damage to the teeth used as abutments for the bridge.
Removing healthy tooth enamel to accommodate a fixed bridge can weaken the structural integrity of the supporting teeth and compromise their long-term health. Once the enamel is removed, it cannot be replaced, leaving the teeth more vulnerable to decay, sensitivity, and potential fractures. This reduction in tooth structure can significantly impact the lifespan of the supporting teeth, as they may become more susceptible to damage and deterioration over time.
Additionally, the stress and strain placed on the supporting teeth by the fixed bridge can lead to increased wear and tear, further shortening their lifespan. The added pressure from chewing and biting can cause the abutment teeth to wear down more quickly, potentially leading to complications such as loosening the bridge or damage to the supporting teeth.
On average, fixed bridges are expected to last 10 to 12 years before needing to be replaced or repaired. However, the lifespan of a fixed bridge can vary depending on factors such as oral hygiene practices, diet, and the overall condition of the supporting teeth and surrounding oral structures. Over time, the cumulative effects of stress, wear, and potential complications associated with fixed bridges can contribute to the loss of the supporting teeth, necessitating further dental intervention and treatment.
It is essential for individuals considering fixed bridges to weigh the potential risks and benefits of this treatment option and discuss any concerns with their dentist. Regular dental check-ups and maintenance are crucial for monitoring the condition of fixed bridges and supporting teeth to ensure long-term oral health and function.
In Conclusion
Neglecting to replace lost teeth can have far-reaching consequences beyond cosmetic concerns. Each tooth in the mouth plays a crucial role in maintaining proper dental alignment and balance. When a tooth is lost and not replaced, the surrounding teeth must compensate for the gap, resulting in an uneven distribution of chewing forces. This uneven distribution increases strain on the remaining teeth during chewing and biting, as they must bear a more significant workload.
The augmented chewing forces can gradually escalate, especially if multiple teeth are missing, causing the remaining teeth to endure excessive pressure. This chronic overload on the adjacent teeth can lead to various oral health issues, including increased risk of tooth mobility, periodontal disease, and tooth fractures. The enhanced strain on the teeth can compromise their structural integrity and make them more susceptible to damage and degradation.
As the remaining teeth attempt to compensate for the missing teeth, they may shift out of their optimal positions, leading to dental alignment and bite function changes. This can result in bite misalignment, jaw issues, and potential complications with chewing and speaking. Additionally, the bone that once supported the missing teeth may start to resorb or diminish in the absence of tooth roots, compromising the remaining dentition’s stability and health.
Ultimately, neglecting to address tooth loss and leaving gaps in the dentition can harm oral health and overall well-being. It is important to seek timely treatment and replace missing teeth to prevent the potential long-term consequences of doing nothing. By restoring the missing teeth with appropriate dental restorations such as dental implants, bridges, or dentures, individuals can maintain proper dental function, preserve oral health, and prevent further complications associated with untreated tooth loss.
If you have questions or need additional information, please Contact Us or Request a Quote to send us your dental inquiry, and we’ll get back to you.